Advanced Treatment for Cerebral Palsy
Selective Percutaneous Myofascial Lengthening (SPML)
Discover a groundbreaking approach to improving mobility and reducing spasticity in cerebral palsy patients.

Innovative Medical Procedure
Understanding SPML
Thousands of clinical trials are conducted and scientific articles are published every month that attempt to improve healthcare and medical research quality by proposing new treatment & diagnostic methods for disorders that affect millions of people worldwide. Selective percutaneous myofascial lengthening is one of the methods for the treatment of cerebral palsy.
Cerebral palsy symptoms and conventional treatments

Cerebral palsy (CP) refers to a group of neurological disorders that appear in infancy or early childhood and permanently affect body movement and muscle coordination. Symptoms can vary widely between individuals, but the main symptoms observed are the following:
Ataxia, including ataxic gait, trouble walking, and uncoordinated movements
Spasticity and muscle tremors
Drooling
Weakness in extremities
Speech and developmental issues, including delays and miscoordination
Typical therapies proposed for CP range from physical rehabilitation to medication and surgical intervention. One procedure which is known to help with this condition is called selective dorsal rhizotomy (SDR): nerve endings are cut only in specific places where spasticity is observed, in order to induce relaxation and pain reduction. It is usually used after other treatment methods have failed and only with optimal patient selection wherein spasticity is the main problem, as opposed to dystonia for example, for diplegic and some quadriplegic patients between the ages of 3 and 9 years. However, it is a proven technique that has evolved for decades into a staple in neurosurgery for the treatment of CP.
SPML as a proposed method of CP spasticity treatment
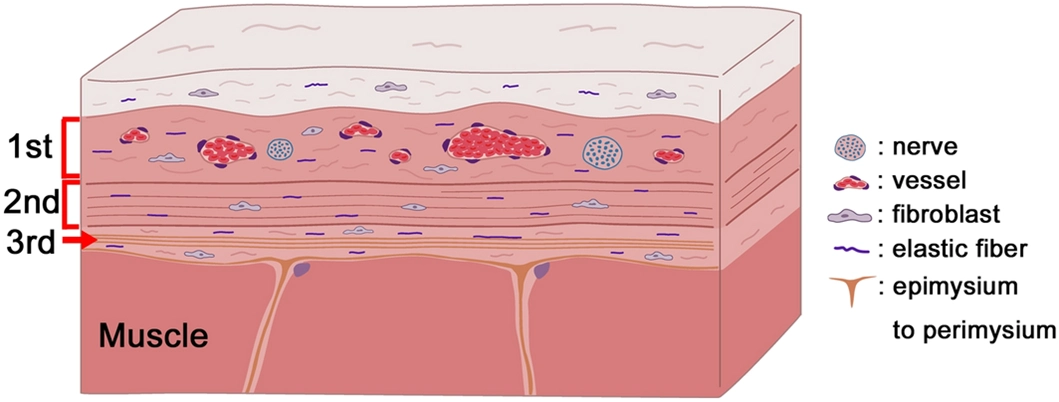
Here comes the new proposed method: selective percutaneous myofascial lengthening (SPML). It works by lengthening certain muscles in order to improve the movement ability of children with CP to sit, stand, or walk; more specifically, small incisions are made through the skin to reach the surface of the muscle that is not long enough. The procedure can be performed on different muscles which are selected based on where the child experiences spasticity. Some medical literature that introduces this procedure indicates that it holds some promise, and the procedure is already being promoted as a promising method on the market.
Standardized intraoperative surgical procedures includes:
Supine positioning of the child
Determination of the areas for the incisions
(which are usually the gastrocnemius, the hamstring, or the hip adductor)
Determination of the palpably tight structures by location and name
Performance of the release surgery
Continuous assessment of the tension over the range of motion
as the release was being performed to prevent over-lengthening
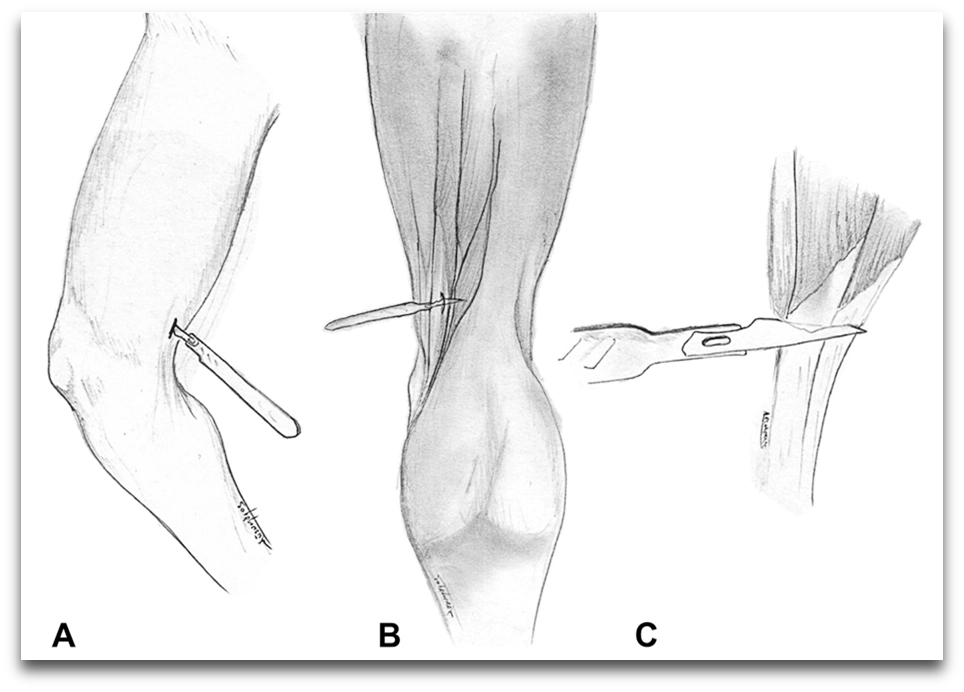
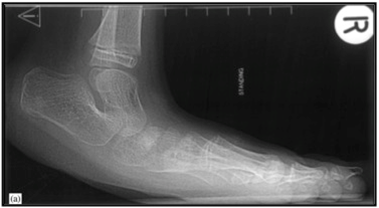
More specifically, gastrocnemius myofascial lengthening is typically performed in the low calf at the distal level of the muscle belly; hamstring surgery includes 1 to 4 of the following as indicated through clinical examination: semitendinosus tenotomy, myofascial lengthening of gracilis, semimembranosus, and biceps femoris (the level of surgery is in the distal third of the thigh, usually within several centimetres of the popliteal crease); and hip adductor tenotomy is performed close to the groin crease. Obturator nerve blocks are used if the child is demonstrating a scissoring gait pattern, the child is reactive to adductor stretch, or if hip dysplasia is evident on anteroposterior pelvis radiographs. The obturator nerve block is typically performed using 3mL of 50% ethanol under ultrasound guidance to increase safety and efficacy. This concentration of ethanol is a relatively gentle agent compared with phenol. The application of ethanol perineural focal dysmyelination is a logical part of this method as it targets dampening of reflexive abnormal movements.
When performing release surgery (or other kinds of minimally invasive surgery), the guiding principle is, “When in doubt, do less. ”We are able to perform this surgery at Saint Luke’s Hospital in Thessaloniki, Greece, with the help of our partnering orthopaedical surgeon, Dr Themistocles Tzatzairis from TheMIS Greece, and his medical team. This procedure should be performed upon request and with proper clearance from a medical professional after examining our other options for treating CP as well.
Limitations of the surgery
While SPML seems to hold the positives of being a minimally invasive surgical technique (namely a “keyhole surgery”), not requiring inpatient post-operative care, and not inducing scarring, it also seems to have significant limitations and relatively little evidence of efficacy.
For starters, it seems to be the case that few, superficial muscles are the ones that can be safely operated on using SPML, meaning that other ones that are located more medially will not be interfered with. However, since the causation of spasticity is not entirely dependent on muscle location, this limitation of the procedure is rather significant in terms of treatment effectiveness. Furthermore, due to it being a keyhole surgery, the surgeon does not directly see what is being cut at any given moment, which is a prominent risk factor for the causation of complications and the limitation of surgery effectiveness too. This is different from conventional open surgery, where the medical personnel has direct visual access to the site of the operation; this is the case with well-known procedures like gastrocnemius release and Achilles’ tendon release. Sadly, to our knowledge, there are no studies that compare these two methods to each other.
As for the evidence that SPML works, the most important studies that speak in favour of it are done without any control groups, which unfortunately makes them unreliable, because medical professionals cannot know whether the effects observed in these studies are due to the procedure itself or miscellaneous independent variables& environmental factors. Also, the articles in question don’t seem to be peer-reviewed, which is another strong blow to their credibility, at least until they are properly reviewed by other medical researchers. Even within the framework of the articles themselves, though, effectiveness of treatment does not seem to be too high. This is evidenced by the fact that, in one study, children manifest no gait improvement and only certain quality of life indicators are improved, such as the socio-emotional aspect of life with CP; while in another study, 10% of the patients needed the surgery to be performed again and a few individuals eventually did need inpatient care afterwards.
In conclusion, for the reasons of a lack of studies comparing SPML to well-established surgical treatments of CP, little evidence in favour of its beneficial effects on child patients, the methodological inadequacy of the studies available on the matter, and concerns over the safety of the procedure, we cannot recommend this procedure to our patients before the evidence rolls in favour of it, let alone without exhausting all other options for them, including SDR and other treatments that are known to help CP children today.
Sources:
- Cerebral Palsy: Diseases and Conditions. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/symptoms-causes/syc-20353999
- Cerebral Palsy: Diagnosis and Treatment. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/diagnosis-treatment/drc-20354005
- Selective dorsal rhizotomy for the treatment of spasticity in cerebral palsy children aged 3-9 years. NHS England. https://www.england.nhs.uk/wp-content/uploads/2019/03/Selective-dorsal-rhizotomy-for-the-treatment-of-spasticity-in-cerebral-palsy-children-aged-3-9-years.pdf
- Steinbok, P. (2007). Selective dorsal rhizotomy for spastic cerebral palsy: a review. Child’s nervous system, 23, 981-990.
- Wild, D. L., Stegink-Jansen, C. W., Baker, C. P., Carmichael, K. D., & Yngve, D. A. (2020). Minimally invasive SPML surgery for children with cerebral palsy: program development. Minimally invasive surgery, 2020(1), 5124952.
- SPML Greece. https://spml.eu/
- Is Selective Percutaneous Myofascial Lengthening an Effective Treatment for Children with Cerebral Palsy? Peninsula Cerebra Research Unit, University of Exeter. https://www.pencru.org/media/universityofexeter/medicalschool/subsites/pencru/pdfs/WTE_SPML_for_publication.pdf
- Yngve D. (2016) SPML Frequently Asked Questions.https://www.utmb.edu/Ortho/Faculty/Yngve.aspx
- Nuzzo, R. Percutaneous Lengthening.http://www.pediatric-orthopedics.com/Treatments/Muscle_Surgery/Perc_Lengthening/perc_lengthening.html


